Georgia's mistakes led the state and federal governments to make duplicate payments for care of some Medicaid patients, a new audit says. Now, Georgia is being asked to refund the federal government's share of the duplicate payments -- more than $665,000.
The over-payments happened because the Georgia Department of Community Health mistakenly issued multiple Medicaid ID numbers to hundreds of patients, says the report by the Office of Inspector General for the U.S. Department of Health & Human Services.
Georgia pays managed care organizations a monthly fee to ensure that Medicaid patients, such as those in the children's health program PeachCare, had access to medical services, so the duplicate ID numbers resulted in duplicate payments, the OIG reports.
The OIG sampled payments for 100 patients, and found the state had made multiple managed care payments for 72 of the patients.
Credit: Lois Norder
Credit: Lois Norder
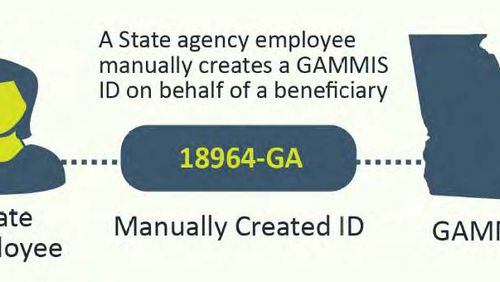
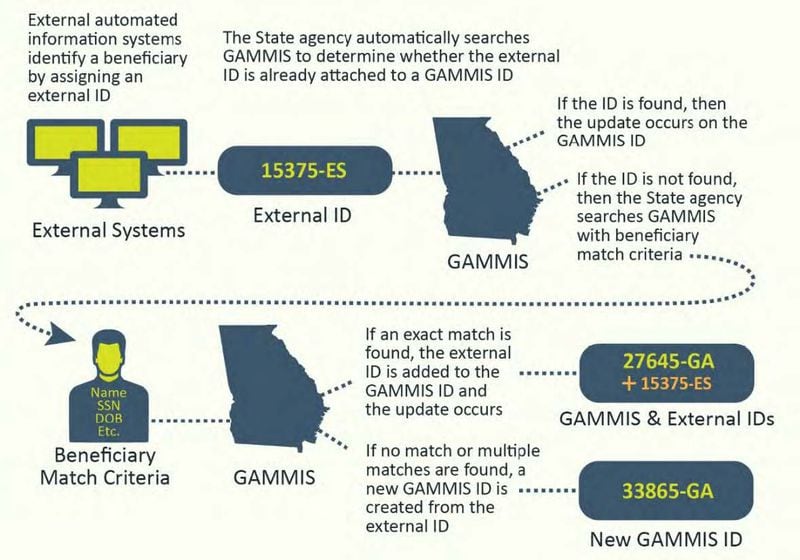
How did the mistakes happen? In part because DCH used several systems to assign Medicaid ID numbers, and when it identified patients with multiple numbers, it didn't properly correct them.
In response to the audit, Georgia Medicaid Chief Blake T. Fulenwider said in a letter to the OIG that it had known of the problem of duplicate numbers since 2006.
Back then, he wrote, DCH implemented a program to try to address the problem. While Fulenwider described that program as "robust," he also wrote that the agency recently took additional steps to root out duplicates.
Credit: Lois Norder
Credit: Lois Norder
Last summer, he wrote, a new integrated eligibility system called Georgia Gateway became operational statewide. "This streamlined approach to issuing (numbers) will significantly reduce the creation of duplicates," he wrote.
DCH may have already recovered and refunded the federal portion of some over-payments, he wrote. The agency will work to determine if other federal money should be refunded, he said.
This is the second time in recent months that the federal inspector general has cited DCH for shortcomings. In September, an OIG report said that Georgia nursing home patients who could be at imminent risk of serious injury or death could not rely on the state to immediately investigate. Georgia took 15 days or more to send an investigator, the report said. Only one state -- Tennessee -- was worse.
Read about that report and how DCH has dealt with the issue here: http://www.ajc.com/news/state--regional-govt--politics/georgia-slow-investigate-when-nursing-home-patients-may-risk/hoqUKrJrxGsXuBZdCEXhGI/