Obamacare mandates it. The feds gave state health agencies eight years to get it done. But with a deadline days away, Georgia still hasn’t posted all the required records online that could help families steer clear of the worst nursing homes.
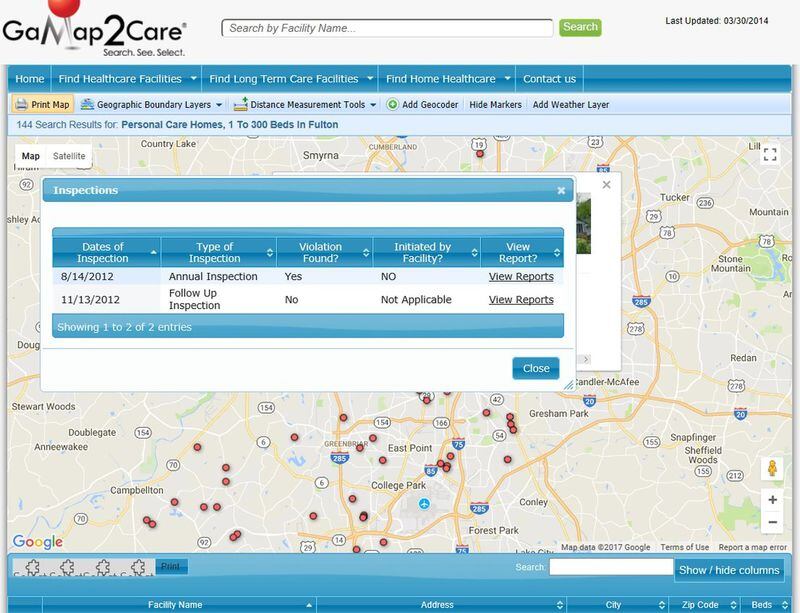
A little-known provision of the Affordable Care Act requires every state to have a user-friendly website with links to enforcement records for every skilled nursing facility that takes Medicare or Medicaid — which is the vast majority. The law specifies that inspection reports, complaint investigations and plans of correction be included.
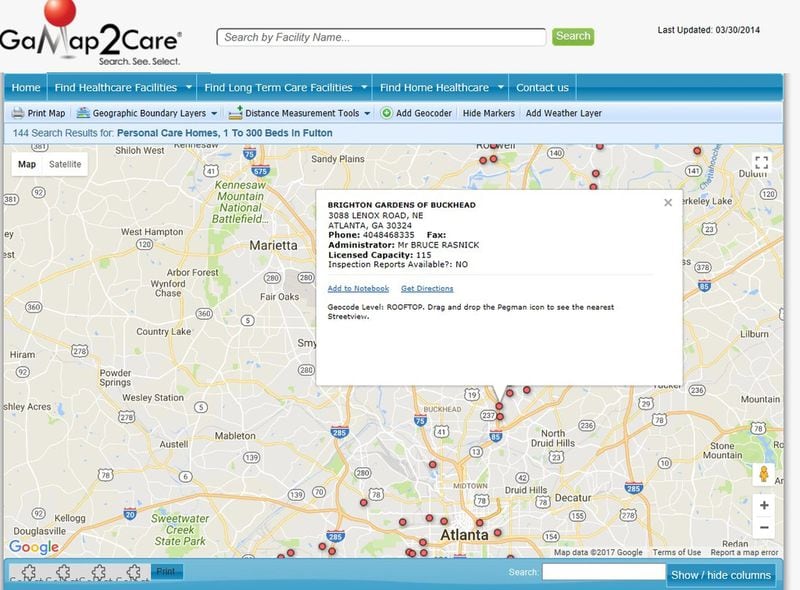
As recently as last week, the Georgia Department of Community Health, which has the job of posting the records, was insisting that its website already met federal requirements, even though information online was riddled with gaps. In some cases, the site linked to inspection records that were three to five years old. For others, the site offered nothing beyond a care home's capacity, the administrator's name, and driving directions.
Some improvements were being planned, a DCH spokeswoman said, but they wouldn’t come until next summer. “We are in the process of improving it as well with an IT vendor,” Fiona Roberts said in an email. “The site should have some additional features available on it by summer.”
But after the AJC raised questions about the Jan. 1 deadline and the federal requirements, the department suddenly reversed course. On Monday, Roberts in an email said that “technical difficulties” are to blame for the dearth of inspection records. On Tuesday, some 2016 and 2017 inspection records had shown up, though for some the links led to error messages or to the federal nursing home website.
Roberts said the IT vendor is working to have up-to-date reports and corrective plans available by New Year’s Day “provided that there are no additional technical issues.”
DCH also will be adding links to the state’s long-term care ombudsman and its aging and disability resource center, she said. The Centers for Medicare and Medicaid Services last year said those were among the new requirements.
The Georgia department, which until this year was grappling with a backlog of inspections and investigating abuse and neglect reports, declined to make the official overseeing the project, or anyone else, available for an interview.
Even with DCH now scrambling to meet the law, Georgia will be among the last states to comply.
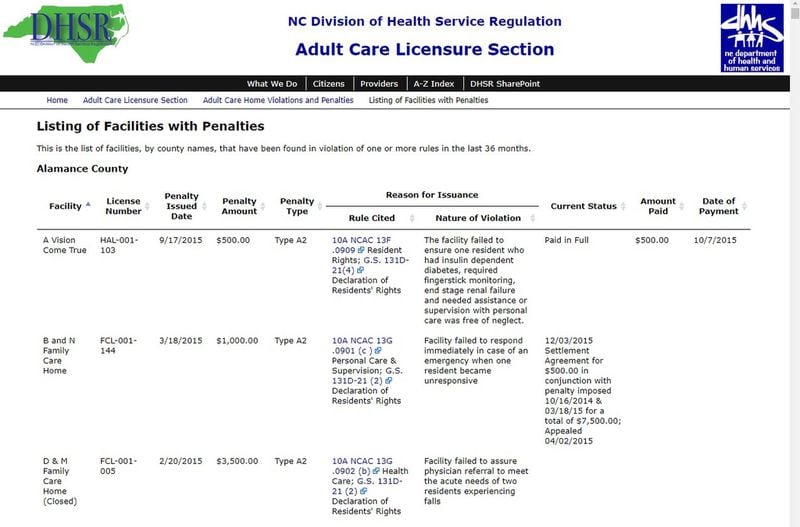
Many states provided inspection and complaint reports on their websites years ago, and some have even included information that the federal government only encouraged them to provide, such as records of fines and sanctions.
About a half dozen other states are also lagging in meeting the requirements, a review by the AJC found, but most of those states said early this month that they were working to meet the deadline. Louisiana was the exception, where officials said they thought they had complied by providing a link to the federal nursing homes website.
A fight for transparency
The Affordable Care Act provision came about after years of efforts in Congress to strengthen oversight and increase information available to consumers and regulators about nursing home quality.
While people trying to find long-term care can look at inspection reports posted on the federal Nursing Home Compare website, patient advocates say it lacks key information. Inspection records are not complete, and the federal site doesn't include corrective action plans.
The state websites are supposed to fill in those gaps, according to Janet Wells, who helped push for the ACA provision in her prior role as public policy director of the National Consumer Voice for Quality Long-Term Care.
“I don’t know why a state would not want to do this anyway, the basics of providing people information,” said Wells, now a policy consultant with California Advocates for Nursing Home Reform.
In theory, posting inspection and investigation records will give people considering where to place an ailing parent or spouse a way to find out quickly if a facility has a history of abusing, neglecting or over-medicating patients, allowing filth to accumulate in rooms or committing other state and federal violations.
"All of a sudden you're in family mode, and it's a crisis," said Melanie McNeil, Georgia's long-term care ombudsman. "I think most people don't plan ahead, don't look at, 'Oh, gosh, I might be in a nursing home in a year or two, let me just search up on that.'
“So being able to just Google long-term care options and pull up a really robust website would be so helpful,” McNeil said.
Such online information might have helped Cheryl Bischof, who unwittingly put her husband of 40 years in one of the most troubled nursing homes in Georgia.
In 2011, John Bischof was lying in a neurointensive care unit, unable to walk, communicate or feed himself, when the hospital gave Cheryl three days to find a rehab center that would take him.
The couple hadn’t planned for this. A few weeks earlier, before a fall in their home and a traumatic brain injury, her husband had been healthy enough to go on neighborhood walks. Afterward, she turned to neighbors to help research nursing homes. She used the phone book. She searched the web. She paid visits to facilities.
Bischof picked a rehab center on Johnson Ferry Road because it was close to the hospital. She knew little about Northeast Atlanta Health and Rehabilitation Center. “It was just, sort of, a decision,” she said, “and it was a bad one.”
Deciding in a vacuum
Northeast Atlanta is currently one of two nursing facilities in Georgia on a federal watchlist for having a history of serious failures, including abuse allegations and improper medical care. In 2016, Northeast Atlanta paid more than $813,000 in federal fines. It was in the news last month when video surfaced of a dying patient repeatedly calling for help, saying he couldn't breathe, and nurses laughing and failing to take life-saving measures as they tried to start his oxygen machine.
Bischof said that during her husband’s brief time there in 2011, instead of putting him in a private room as she requested, the staff put him in a locked ward in the basement.
"One night they called and they said, 'Your husband's on the floor,'" she said. "And I said, 'Well why don't you get him up off the floor? Why are you calling me?' 'Well we think you need to come down here and try to calm him.' It was atrocious."
The director of Northeast Atlanta, which is under new management, did not return a call from The Atlanta Journal-Constitution.
Over the next six years John Bischof would shuffle between nursing homes, hospice care and home care, costing the family $620,000 out of pocket. He died earlier this year from sepsis caused by a bedsore, which his wife blames on another nursing facility.
“I have had people all the time say, ‘What should I do, where should I go?’” Bischof said. “And I cannot say anything good. Like how to start. How do deal with it when you’re there. It’s a bad situation.”
Weakened regulation
Under federal law, states that shirk the new website requirement could have Medicare and Medicaid funds withheld. But patient advocates question whether CMS, in the deregulation climate created by President Trump, will make a priority of making public what could be embarrassing details about the long-term care industry.
So far this year, CMS has been seeing things the industry's way. For example, earlier this year the agency rejected a ban on binding arbitration agreements that long-term care facilities can force families to sign. Such agreements can shield nursing homes from lawsuits if a loved one is abused, sexually assaulted or neglected.
“There is a real effort to weaken how nursing homes are inspected and the enforcement,” said Robyn Grant, policy director of the National Consumer Voice for Quality Long-Term Care.
And the nursing home lobby is powerful. In Georgia nursing home owners have been among the biggest political donors to state parties and candidates, including Gov. Nathan Deal and Lt. Gov. Casey Cagle. The Georgia Health Care Association, nursing homes' lobbying arm, hired Deal's son-in-law just after he was elected in 2010, as well as House Speaker David Ralston's niece.
» AJC Exclusive | Lax oversight leaves patients at risk in Medicaid rides program
The association said it didn’t know enough about the federal government’s requirements, nor the state’s plans to comply, to comment.
“GHCA will always be supportive of transparency and the availability of accurate information for consumers to assist with decisions in regards to skilled nursing care for their loved ones or themselves,” a spokesman said in an email.
David Wright, CMS’s survey and certification director, said in an emailed statement that the agency will inventory state websites after Jan. 1 and evaluate them for compliance with the federal law as well as utility for consumers.
“States that do not have compliant websites by Jan. 1, 2018 will be required to provide an action plan to their CMS Regional Office on how they intend to meet this requirement,” he said.
Improving nursing homes
Along with requiring states to provide more information about nursing home quality, the Affordable Care Act set new requirements for oversight. Under the law, nursing homes and other long-term care facilities that receive federal funds must:
- disclose detailed information about who owns or manages their operations;
- establish programs to prevent and detect criminal, civil and administrative violations;
- report suspected crimes against residents to law enforcement and to the state survey agency.
About the Author