A new cancer treatment experiment at Stanford University that used immune-stimulators to target tumors in mice had remarkably encouraging results.
After injecting a combination of two immune boosters directly into solid mouse tumors, the research team said the vaccination eliminated all traces of the specifically targeted cancer from the animal’s entire body — including metastases that were previously untreated.
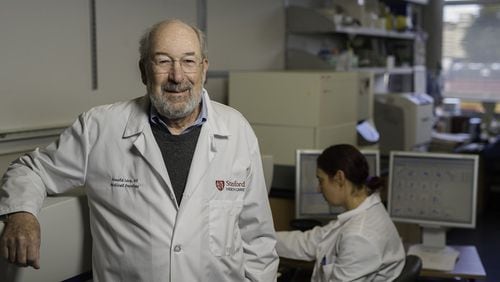
“When we use these two agents together, we see the elimination of tumors all over the body,” senior author of the study, Dr. Ronald Levy told the Stanford Medicine News Center. “This approach bypasses the need to identify tumor-specific immune targets and doesn’t require wholesale activation of the immune system or customization of a patient’s immune cells.”
Out of the two immune “agents” used in the study, published in the journal Science Translational Medicine, one has already been approved for use in humans and the second is currently involved in a lymphoma treatment trial.
The study explained that when an immune system detects cancer cells in the body, its T cells attack the tumor but, over time, the tumor devises ways to overpower the immune cells and continues to grow.
In Levy’s experiment, the cancer-fighting T cells from the immune system were rejuvenated when a microgram (one-millionth of a gram) amount of the two immune boosters was injected into a mouse’s lymphoma tumor. Those same cells then moved on from the tumor it destroyed to find any other identical cancers in the body. Although the injection was successful in eliminating the targeted tumors present in the mouse, the T cells did not move on to a colon cancer tumor also found in the animal.
“This is a very targeted approach,” Levy said. “Only the tumor that shares the protein targets displayed by the treated site is affected. We’re attacking specific targets without having to identify exactly what proteins the T cells are recognizing.”
The experiment was replicated in 90 other mice and was successful in eradicating the tumors in 87 of them, allowing the researchers to declare them cancer-free. The cancer did recur in three of the animals, but the tumors later regressed after another round of immune treatment. The study was also successful in mice that had breast, colon and melanoma tumors.
“I don’t think there’s a limit to the type of tumor we could potentially treat,” Levy said, “as long as it has been infiltrated by the immune system.”
Unlike other cancer treatments already on the market, this method negated the need to infiltrate the animal’s whole immune system or use samples from its body. In some cancer therapies that already exist, like T-cell treatment used to combat leukemia and lymphoma, the patient’s immune cells need to be removed from the body and then are genetically altered to fight the cancerous cells before being reintroduced to a person’s system. This method is expensive, involves a lengthy treatment process and comes with a battery of rough side effects. But the new method is simpler.
“All of these immunotherapy advances are changing medical practice,” Levy said. “Our approach uses a one-time application of very small amounts of two agents to stimulate the immune cells only within the tumor itself. In the mice, we saw amazing, body-wide effects, including the elimination of tumors all over the animal.”
About the Author